We’ve all seen the headlines. “Segmented Sleep: The Secret History of Rest!” “Biphasic Sleep: Unlock Your Productivity!” The allure of dividing your night into two four-hour chunks, maybe with a productive or meditative interlude, is powerful. It sounds ancient, natural, and efficient. But before you swap your eight-hour block for two shorter “shifts,” we need to have a serious conversation about what’s happening inside your body, specifically concerning the delicate dance of melatonin and the symphony of endocrine hormones.
Is Segmented Sleep a Historical Gem or a Hormonal Hazard?
The historical argument for segmented sleep (often called “biphasic” or “polyphasic” sleep, though the true historical pattern was typically just two segments separated by an hour or two of waking) suggests our ancestors naturally slept this way before artificial light dominated the night. While compelling, this historical perspective often bypasses one crucial modern factor: biology hasn’t changed, but our exposure and environment have.
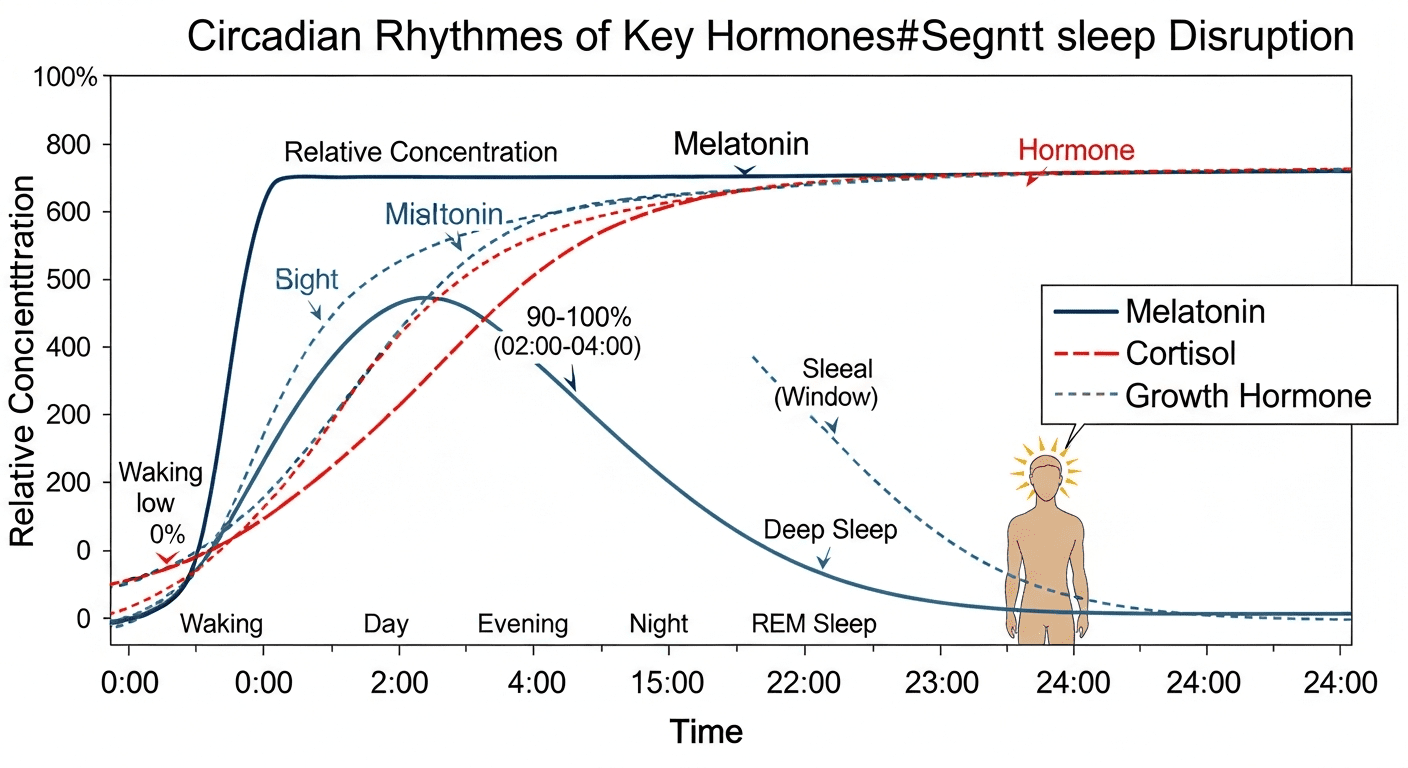
Today, when we attempt to mimic the segmented patterns of the 16th century, we are doing so under the glare of screens, LED lights, and 24/7 stress. This intervention fundamentally disrupts the core mechanism regulating sleep: the circadian rhythm, which relies heavily on the uninterrupted flow of melatonin and the sequential release of essential hormones like Cortisol and Growth Hormone (GH). This is where the historical romanticism of segmented sleep crashes headfirst into modern endocrinology.
The Melatonin Misalignment Problem: Why the Gap Matters
Melatonin, often dubbed “the hormone of darkness,” is far more than just a sleep trigger. It is a critical synchronizer for almost every physiological process. Its levels begin to rise dramatically about two hours before habitual bedtime (the Dim Light Melatonin Onset, or DLMO) and should peak in the middle of the night before tapering off before dawn.
The Light Gap and Phase Delay
In a segmented sleep pattern, you intentionally wake up—usually after 3 to 4 hours—and engage in activities. This is the crucial mistake. Even if you keep the lights low, exposure to modern light sources (especially blue and green wavelengths) during the “waking gap” dramatically suppresses melatonin production. Researchers define a “significant suppression” as even brief exposure to standard indoor lighting.
- The Suppression Effect: Even relatively dim light (around 50 lux, typical hallway lighting) can halve melatonin output.
- The Phase Shift: When melatonin is suppressed mid-cycle, it effectively tricks the Suprachiasmatic Nucleus (SCN)—our master clock—into believing it is still daytime. This causes a phenomenon called circadian phase delay.
- Impact on Second Sleep: If your DLMO is pushed later, the second sleep segment begins out of sync with your body’s true biological clock, making it harder to fall into the critical deep stages of sleep necessary for cellular repair and hormonal cycling.
Think of it like trying to conduct an orchestra, but every time the bassoon section hits its peak, you blast a loud air horn. The conductor (your SCN) gets confused, and the timing of the entire performance is ruined.
Measuring the Melatonin Nadir and Sleep Inertia
The deepest, most restorative sleep occurs when melatonin is peaking—the melatonin nadir. Segmented sleeping forces an unnecessary waking during this critical peak. When you try to transition back into the second sleep segment, your body is fighting the recent light exposure and the lingering effects of the first sleep cycle. This often results in fragmented, shallow second sleep characterized by increased sleep inertia—that groggy, slow-to-start feeling.
Furthermore, the total duration of high melatonin levels is paramount for its protective, antioxidant, and immunomodulatory functions. By segmenting sleep and introducing light gaps, you reduce the overall time your body spends saturated in protective melatonin, potentially impacting long-term health markers.
The Deep Sleep Dilemma: Growth Hormone, Cortisol, and Segmented Fragmentation
The circadian system doesn’t just manage when you sleep; it dictates what happens while you sleep. The release of major metabolic and stress hormones is tightly choreographed to the stages of the sleep cycle. Segmented sleep often interferes with the sequential cycling necessary for optimal hormonal output.
The Crucial Release of Growth Hormone (GH)
Growth Hormone is not just for children; in adults, it is essential for muscle repair, fat metabolism, bone density maintenance, and overall vitality. Approximately 60–70% of the daily GH pulse occurs during the first few hours of the night, specifically synchronized with the deepest stages of Non-REM sleep (Slow-Wave Sleep or SWS).
If you implement a segmented sleep schedule, the first segment typically captures this vital SWS phase, which sounds positive. However, fragmentation and interruption significantly diminish the quality and quantity of SWS. When you introduce a waking period, even a short one, the subsequent attempt at sleep often struggles to achieve the same deep SWS penetration, meaning the remaining GH release is less effective or absent.
Impact: Chronic disruption of SWS due to segmentation can lead to lower GH output, potentially contributing to slower recovery, reduced metabolic rate, and impaired body composition over time.
Cortisol’s Pre-dawn Surge and the Interruption Danger
Cortisol, the primary stress hormone, has a beautiful and necessary rhythm. It is at its lowest (the nadir) around midnight, allowing the body to rest and repair. It then begins its natural, gentle climb, peaking sharply just before and upon waking (the Cortisol Awakening Response, or CAR), giving you the energy needed to face the day.
The problem with segmented sleep’s second half—which often occurs in the pre-dawn hours (e.g., 4:00 AM to 8:00 AM)—is that it perfectly aligns with the natural cortisol surge. If your fragmented pattern causes stress or anxiety about “getting back to sleep,” or if you engage in demanding activities during the middle wake period, you risk spiking cortisol prematurely.
“The biological timing of sleep is everything. When we interrupt the restorative phases, especially the REM-heavy segments later in the cycle, we disrupt the delicate feedback loop between the HPA axis (Hypothalamic–Pituitary–Adrenal) and the immune system. Segmented sleep, unless performed in a perfectly controlled, dim environment, is essentially introducing a mini-stressor during a biologically critical window.” – Dr. Alistair Jenson, Sleep and Endocrine Researcher.
Elevated cortisol later in the night inhibits the deep sleep (SWS) that the body might still need and prevents the smooth transition into the final REM cycles—which are crucial for emotional processing and memory consolidation. This hormonal mismatch contributes to the feeling of waking up “tired but wired.”
Metabolic Mess: Insulin, Ghrelin, and Leptin
It’s not just the major endocrine regulators that suffer; the hormones governing your metabolism and appetite are also tightly coupled to continuous, quality sleep. Segmented sleep often leads to chronic partial sleep deprivation, even if the total hours accumulated are 7 or 8 hours. The fragmentation itself is the problem.
Insulin Resistance and Segmented Stress
When sleep is fragmented or restricted, the body’s sensitivity to insulin decreases significantly. Studies show that even a few nights of interrupted sleep can push healthy individuals toward a pre-diabetic state. Why? Sleep loss elevates norepinephrine, which increases glucose production. If you are awake mid-cycle and potentially snacking (a common habit in segmented sleep schedules), you are introducing carbohydrates when your body’s hormonal signals are least equipped to manage them, spiking blood sugar and increasing the likelihood of chronic insulin resistance.
Appetite Dysregulation: Ghrelin and Leptin Imbalance
Sleep deprivation dramatically alters the levels of ghrelin (the hunger hormone) and leptin (the satiety hormone). Segmented sleep can mimic the effects of sleep restriction because the body perceives the fragmentation as stress. Specifically:
- Ghrelin Increases: You feel hungrier, particularly for high-calorie, sugary foods.
- Leptin Decreases: You never feel truly full, leading to overconsumption.
The waking period in the middle of the night—especially if it involves light and activity—is a potent trigger for ghrelin release, driving late-night hunger and contributing to long-term weight gain and metabolic syndrome.
Data Comparison: Monophasic vs. Segmented Sleep and Hormonal Health
To truly appreciate the biological cost, we must compare the optimal hormonal environment created by continuous sleep versus the disrupted environment of a segmented schedule.
| Hormone/Factor | Optimal Monophasic Sleep (7-9 hours continuous) | Segmented Sleep (Two 4-hour segments) | Impact of Disruption |
|---|---|---|---|
| Melatonin Peak (Nadir) | Sustained peak for 4-6 hours, signaling darkness and repair. | Suppressed by light exposure during the middle waking period, leading to a flatter, shorter duration. | Compromised antioxidant function; phase delay; difficulty initiating second sleep. |
| Growth Hormone (GH) | Massive pulse during the first 90 minutes (SWS). | Initial pulse may occur, but subsequent SWS required for further pulses is often shallow or missed due to fragmentation. | Reduced physical recovery, impaired muscle repair, decreased metabolic rate. |
| Cortisol | Lowest levels (nadir) maintained until 3-4 AM; sharp rise upon waking (CAR). | Often spikes during the middle wake period (due to stress/light); blunts the necessary sharp rise later, leading to fatigue. | Increased HPA axis activation; “tired but wired” feeling; heightened anxiety. |
| Insulin Sensitivity | High sensitivity maintained throughout the sleep cycle. | Significantly reduced sensitivity (mimics partial sleep deprivation), especially if consuming food during the gap. | Increased risk of insulin resistance and Type 2 diabetes over time. |
| Appetite Hormones (G/L) | Balanced: High Leptin (satiety), Low Ghrelin (hunger). | Imbalanced: Low Leptin, High Ghrelin, driving cravings and overeating. | Metabolic dysfunction and propensity for weight gain. |
Why the Biphasic Bias Persists: Romanticism vs. Rigor
If the biological data so clearly favors continuous, monophasic sleep (or carefully controlled biphasic sleep that aligns with natural light, like a siesta), why does segmented sleep still have its advocates? Primarily, the arguments are driven by historical romanticism and the desire for perceived productivity.
The False Promise of Extra Time
The primary draw is the idea of gaining a productive, quiet hour or two in the middle of the night. However, this productive gap often comes at the expense of cognitive function during the day. When hormones are regulated correctly, you gain energy and focus during the day that far outweighs the limited output achieved during the biologically challenging midnight hours. Segmented sleep often steals from daytime clarity to pay for midnight fragmentation.
A Note on Natural Naps (True Biphasic Sleep)
It is important to distinguish between disruptive segmented sleep (waking for hours during the melatonin peak) and natural biphasic sleep, such as the Mediterranean siesta. A true, biologically sound biphasic pattern involves a long night segment (5-6 hours) and a short, non-disruptive nap (20-90 minutes) during the natural post-lunch dip (about 7-9 hours after waking). This nap does not interrupt the crucial melatonin nadir or the early-night SWS, making it hormonally safer.
Practical Strategies for Hormonal Harmony
If you genuinely struggle with continuous sleep and find yourself waking naturally mid-cycle, you should prioritize mitigating hormonal damage rather than embracing the fragmentation.
- Minimize Light Exposure (The #1 Rule): If you must wake up, use ultra-dim red light only. Red light has the least impact on melatonin suppression. Avoid all screens (phones, tablets, TVs).
- Keep the Gap Short: If the original segmented sleepers woke for an hour or two, they often stayed quietly in bed, sometimes reading by candlelight. Keep your waking period to less than 60 minutes and avoid stimulating activity.
- Maintain Darkness Discipline: Ensure that the environment you return to for the second sleep segment is perfectly cool, dark, and quiet. Light exposure during the initial rise of melatonin makes your sleep architecture brittle; don’t break it further.
- Focus on Sleep Efficiency: Rather than trying to schedule two perfect segments, focus on maximizing the quality of one continuous block. Prioritize the first four hours of sleep above all else, as this is your GH and SWS window.
Key Takeaways: The Hormonal Cost of Fragmentation
- Melatonin is Light-Sensitive: Modern light exposure during the segmented wake period actively suppresses melatonin, pushing back your circadian clock (phase delay).
- SWS Is Early: Growth Hormone release and the most restorative deep sleep occur primarily in the first 3-4 hours of continuous sleep. Segmentation interferes with subsequent deep sleep recovery.
- Cortisol Rises Late: The segmented schedule often forces waking during the period when cortisol is naturally low or just beginning its surge, leading to premature HPA axis activation and stress.
- Metabolism Suffers: Fragmented sleep mimics sleep deprivation, severely impairing insulin sensitivity and skewing appetite hormones (Ghrelin/Leptin).
- Continuous is King: For optimal endocrine health, prioritize 7–9 hours of continuous, dark, undisturbed sleep aligned with your natural DLMO.
Your productivity depends not on the quantity of time you are awake, but the quality of time you are asleep.
FAQ: Segmented Sleep and Hormones
1. Does the historical precedent of segmented sleep mean it’s naturally better for us?
Not necessarily. While people historically engaged in segmented sleep, their environment was vastly different—no artificial blue light, vastly lower ambient light, and often slower, more meditative waking periods. Our modern attempts rarely replicate these conditions, leading to light exposure and hormonal disruption that our ancestors simply did not face.
2. Can I segment my sleep without affecting my hormones if I avoid light entirely?
It’s extremely difficult. While avoiding blue light helps maintain melatonin levels, the act of becoming mentally alert and physically moving often elevates cortisol and disrupts sleep pressure (adenosine). True hormonal preservation requires you to stay in a state that is almost meditative rest, avoiding any stimulating activity, food, or intense thought. For most people, this is impractical.
3. I naturally wake up at 3 AM. Should I just get up and be productive?
If you wake up, treat it as a temporary interruption, not an opportunity for productivity. Focus on reducing anxiety around the waking, use dim red light, and employ relaxation techniques (deep breathing, meditation). Getting up and being productive reinforces the waking pattern and actively works against your circadian rhythm by suppressing melatonin and prematurely spiking cortisol.
4. How long does light exposure suppress melatonin during the night?
The suppression is immediate, and the recovery is slow. Even brief exposure (5–10 minutes) to bright room light or device screens can push melatonin back significantly, sometimes taking hours for it to rebound to pre-exposure levels. This gap prevents the body from achieving peak restorative function during the later sleep cycles.
5. Is the afternoon nap (siesta) a form of segmented sleep? Is it harmful?
The afternoon nap is a form of true biphasic sleep, and it is generally beneficial if kept short (20–90 minutes) and timed correctly (mid-afternoon). It does not interrupt the crucial, early-night melatonin peak or SWS. It enhances alertness without disrupting the primary overnight restorative functions, making it hormonally safe.
Conclusion: Protecting the Nightly Symphony
The movement toward segmented sleep is often driven by a genuine search for optimizing time and productivity, leveraging a romantic view of history. However, the rigor of modern science clearly shows that in our light-polluted, highly stressed world, segmenting sleep is an endocrine gamble.
By constantly interfering with the natural progression of sleep cycles, we actively sabotage the finely tuned mechanism that regulates melatonin, growth hormone, cortisol, and our entire metabolism. While historical sleepers may have enjoyed their “first” and “second” sleeps, they didn’t have a pocket-sized screen blasting blue light into their eyes at 2 AM.
For sustained health, vitality, and metabolic function, we must stop trying to fight our biology. Prioritizing one long, continuous block of high-quality sleep remains the most powerful tool we have for protecting our hormonal health and maximizing our physical and mental performance when the sun is actually up.
Sleep well, stay synchronized, and let your hormones do their critical work!